The Safety Blog
The Safety Blog serves to highlight patient safety news and stories aimed at upholding our mission: safe care for every patient, every time, everywhere.
PROMOTING SAFETY & QUALITY IN SKILLED NURSING & ASSISTED LIVING FACILITIES
by Elena Madrid, Director of Regulatory Affairs, Washington Health Care Association
How can a state organization help promote patient safety for elderly communities? Elena Madrid shares her experiences from inside the WHCA and the work they do to sustain quality in these indispensable facilities.
About the WHCA
The Washington Health Care Association (WHCA) is a statewide non-profit organization representing over 400 assisted living and skilled nursing facilities. WHCA’s mission is to promote quality long-term and post-acute health care and services, while serving as an advocate for providers, staff, and the patients and residents they care for. Association members provide health and personal care, social support and housing to 25,000 frail, elderly, or disabled Washingtonians each day. About 25,000 employees work for member facilities.
Through its leadership and engagement with federal and state quality improvement initiatives, WHCA and its members are committed to healthy, affordable, and ethical long-term care. In keeping with the continuous evolution of long-term healthcare, our quest for sustained quality improvement in this arena is achieved through active engagement with all stakeholders.
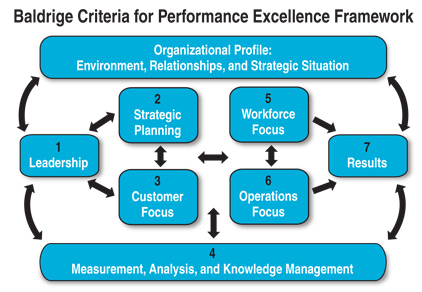
Applying the Baldrige Performance Excellence Framework
The Washington Health Care Association works in conjunction with America Health Care Association (AHCA)/National Centers for Assisted Living (NCAL) to focus on its Quality Initiatives. Our current focus is challenging members to apply the Baldrige Performance Excellence Framework, an approach which was the foundation of the 2015-2018 AHCA Quality Initiative, to meet measureable targets in eight areas with three key priorities focused on improvement in:
- organizational success
- short-stay/post-acute care
- long-term/dementia care
WHCA also works directly with our assisted living and skilled nursing facility members to pursue the AHCA/NCAL National Quality Award Program. The program provides a pathway for providers of long-term and post-acute care services to journey towards performance excellence. It is based on the core values and criteria of the , employing the above framework.
Member facilities may apply for three progressive levels of awards: Bronze—Commitment to Quality, Silver—Achievement in Quality, or Gold—Excellence in Quality. In 2015, six Washington WHCA LTC facilities received the AHCA/NCAL Silver Quality Award and 29 received the Bronze Quality Award, placing Washington in the top five states in the nation for Bronze Awards.
Target Goals: Reducing Readmissions and Antipsychotic Use
One of our target goals is to safely reduce the number of hospital readmissions within 30 days during a skilled nursing center stay by an additional 15% or achieve and maintain a low readmit rate of 10% by March 2018. To accomplish this goal, WHCA assists members through education in the form of conferences, webinars, and written resources. We also serve as support through consultation on regulatory requirements for both assisted living and skilled nursing facilities.
Another target goal relates to safely reducing off-label use of antipsychotics. Studies have shown that antipsychotic medications provide only a small benefit for a limited set of individuals with dementia, but pose a large risk of adverse events (Ballard, Waite, & Birks, 2006; Maher, et al., 2011). In 2012, the CMS launched the national Partnership to Improve Dementia Care in Nursing Homes, which AHCA/WHCA supported, setting the goal of a 15% reduction in use of off-label antipsychotics. WHCA was able to achieve this this goal at the end of 2014, in part by utilizing guest speakers for webinars, conferences, and other events.
In September 2014, CMS along with AHCA and others set new goals, still in motion today, to continue reducing the use of antipsychotic medications. The target is to safely reduce the off-label use of antipsychotics in long-stay nursing center residents by an additional 15% by December 2016. WHCA supports and assists our members to reach these quality goals through provision of resources and ongoing educational opportunities. As an example, two webinars conducted last month touched on this goal – one from Sharon Eloranta entitled Sepsis, Readmissions, and Skilled Nursing Facilities, and another from Sarah Kneisler entitled MCI (Mild Cognitive Impairment) Today, Dementia Tomorrow: Improving Clinical Strategies.
About the Author
Elena Madrid joined WHCA in 2014 as the Director of Assisted Living, Residential Care, and Quality after nearly 16 years with DSHS-Residential Care Services where she was a nursing facility surveyor, complaint investigator, and a field manager responsible for the supervision of the licensors, surveyors, and complaint investigators for assisted living, skilled nursing facilities, and adult family homes in eastern Washington. Elena has also worked as a director of nursing in both assisted living and skilled nursing. She is a registered nurse and brings a wealth of knowledge regarding long term care requirements and the regulatory issues affecting long term care providers. She serves as a regulatory and clinical support person for assisted living and skilled nursing members. Elena spends much of her time focused on assisted living quality and support. Her background in both assisted living and skilled nursing will provide a great resource to all of WHCA members.
DECREASING INFECTIONS IN HEALTHCARE SETTINGS
by Sharon Eloranta, Medical Director, Quality and Safety Initiatives, Qualis Health
At Qualis Health, we are working to decrease healthcare associated infections (HAIs) in hospitals, skilled nursing facilities, and outpatient/ambulatory surgery centers. Healthcare associated infections are relatively rare, but can be devastating to patients and families and costly for the healthcare system and payers. It is clear that different strategies are needed to reduce these infections in different settings, even though the basics of infection prevention are the same throughout the healthcare system.
As an externally-funded consulting organization, Qualis Health is unique in that our services are provided through funding from the Centers for Medicare & Medicaid Services, meaning that our providers work with us voluntarily. As such, our task is to identify what would motivate providers to participate with us – and conversely, what barriers might limit participation. We’ve been able to address most of these barriers by linking healthcare associated infections to pay-for-performance programs and to upcoming rule-making that specifies new expectations for infection prevention programs across various settings.
At the individual hospital and unit level, the defining element for success is strong support at the leadership level – looking at healthcare associated infections as a true patient safety concern.
Luckily for us, offering assistance in meeting these external demands is often successful. However, we also cannot declare victory – infections continue to emerge, and changes on the system level take time to achieve. Continuous vigilance is needed to ensure that preventive measures remain in place. Organizations must continue to monitor problem areas and be ready to intervene if data indicate an emerging problem.
One key issue: In hospitals, the infection preventionists are spread very thin. In order to help hospitals focus this scarce resource, a recent initiative of ours provided reports to help facilities target the individual units within their buildings that are contributing to the highest numbers of infections. This number is compared to what similar units might expect for that infection type on the national scale). We called this the “Wheel of Misfortune,” which prevents the “spray and pray” approach and allows the infection preventionists to deploy targeted interventions at the level that will do the most good. We also championed the use of the related Centers for Disease Control’s Target-Assess-Prevent (TAP) survey, which creates a list of infection prevention processes that are reported by all levels of staff to be highly variable, because variation in practice leads to error.
Another issue is overuse and misuse of antimicrobials leading to the spread of multi-drug resistant organisms, as well as to infections themselves, such as Clostridium Difficile. To address this, we are striving to help providers at all levels of readiness take steps to assess and optimize their antimicrobial use.
The Qualis Health team is also partnering with the Department of Health, chapters of the Association of Professionals in Infection Control (APIC) and others to develop recommendations, resources (such as a workbook) and tools to support antimicrobial stewardship across all healthcare settings.
At the individual hospital and unit level, the defining element for success is strong support at the leadership level – looking at healthcare associated infections as a true patient safety concern.
Outcomes
What were the primary outcomes or impact of this work?
Many of the units we’ve targeted for technical assistance have achieved decreased infections – and many providers are taking steps to optimize antimicrobial use and to create fully functional infection prevention programs (not just infection prevention projects).
What were the largest “lessons learned” in this effort?
We are still working every day to help hospitals, nursing homes and providers in other settings to improve their infection prevention systems and reduce these harms to patients. One major lesson learned is that no matter what the infection is, it’s critical to involve a multidisciplinary team and really dive into the root causes of the infections – throw the doors wide open and examine every nook and cranny. The most successful efforts so far rely on hands-on hard work, done by teams, with respect for every discipline’s role. The “fancy answer” is often not the right one!
What were the reactions of patients, families, and/or staff effected by the work?
Some of the feedback we’ve received:
“You did a wonderful job explaining exactly what I needed in a way that I could understand.”
“[Qualis Health’s] help is so valuable to those of us who want to succeed at having safe/high quality ASCs [Ambulatory Surgical Centers].”
“I especially appreciated [Qualis Health’s] approach of tackling ‘doable” chunks – we have so much to fix in our facility and I often feel overwhelmed. I appreciate the direction provided and especially [the reassurance] of not trying to fix everything all at once.”
“Had not thought to use tracer activity to look at what is going on throughout our facility to really identify areas where we may have gaps.
“Thank you for the information provided in meaningful ways and addressing our unique needs.”
If another organization took on a similar project, what would be your biggest suggestion?
The top considerations in terms of critical resources or barriers:
- Be very knowledgeable about how HAI data is collected and know the data well.
- Use the data to target interventions where they are most needed.
- Convene a multidisciplinary team, with strong leadership support, and empower the team to explore every possible solution.
- Get back to infection prevention basics!
Point of Contact:
Sharon Eloranta
Medical Director, Quality and Safety Initiatives
SHARONE@qualishealth.org
About the Author

Sharon Eloranta provides training and consultation in the field of healthcare quality and is a frequent speaker on quality and safety improvement methods.
Dr. Eloranta has more than 20 years of experience in healthcare, and under her leadership, Qualis Health has conducted multiple local, regional and national collaboratives on diabetes care, primary and secondary prevention of cardiovascular disease, prevention of surgical site infections, and nursing home improvement on pain and pressure ulcers. Dr. Eloranta is a George W. Merck Fellow at the Institute for Healthcare Improvement (IHI).